Steps to Minimize Claim Denials Before Treatment

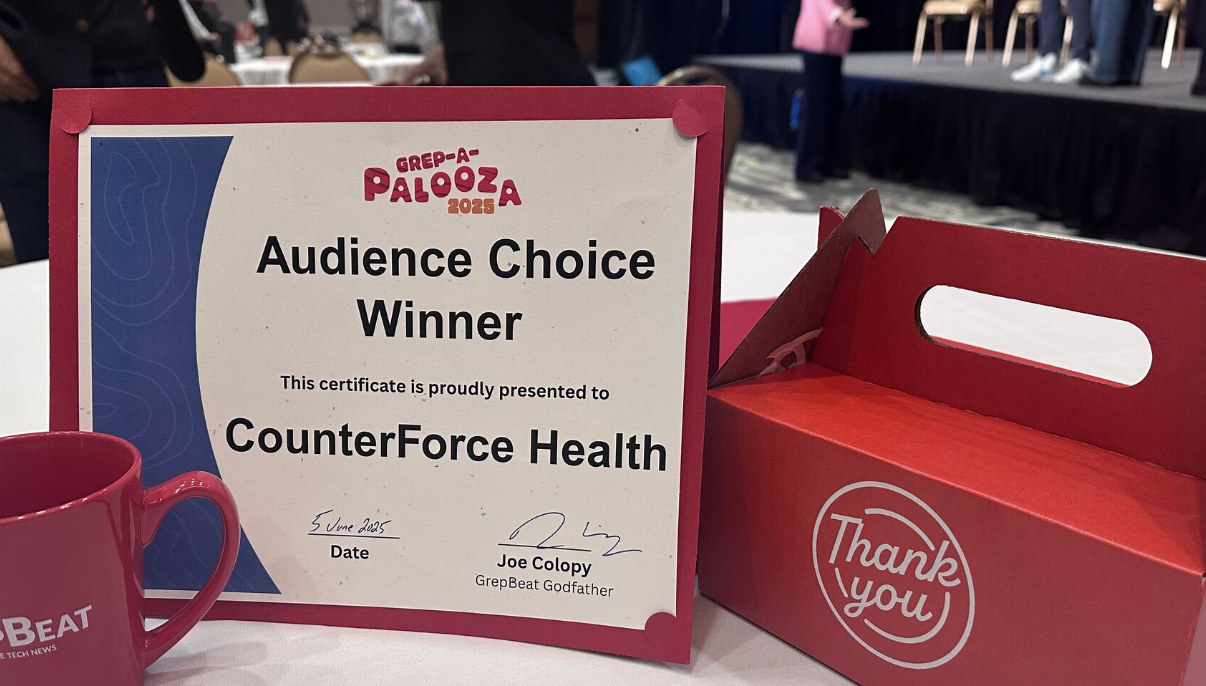
The healthcare journey is often fraught with unexpected turns, and one of the most frustrating is the dreaded health insurance claim denial. While Counterforce Health is here to equip you with powerful tools to fight back after a denial occurs, what if you could take steps to minimize the chances of a denial even before treatment begins?
Shifting from a reactive stance to a proactive one can significantly reduce stress and financial burden. By understanding key aspects of your insurance policy and taking a few crucial preparatory steps, you can navigate the system more effectively and potentially avoid the need for an appeal altogether. This approach aligns perfectly with Counterforce Health's mission to empower patients and reduce the burden of a complex healthcare system, allowing you to focus on healing rather than fighting for coverage.
Here’s how you can empower yourself proactively:
1. Verify Coverage Before Procedures: Your Pre Treatment Checklist
Before any significant medical procedure, medication, or even a specialist visit, it’s vital to confirm your insurance coverage. Don't assume everything is covered just because you have insurance. Many services require specific approvals, and understanding these requirements upfront can save you considerable time, money, and stress down the line.

- Pre-Authorization (Prior Authorization): The Golden Rule of Prevention Many medical services, including certain procedures, medications, and durable medical equipment (DMEPOS), require pre-authorization from your insurance company before you receive them.This means your insurer must approve the service before you receive it. Failing to obtain pre-authorization is a common reason for claim denials.
- What to Do: Always check with your healthcare provider and your insurance company if pre-authorization is needed for any upcoming service. Your provider's office is typically responsible for initiating this process.They have access to lists of services that require prior authorization and can verify your benefits through their provider portals.However, it's crucial for you, as the patient, to be prepared and informed. Ask your provider if they have submitted the pre-authorization request and keep a record of the approval. Proactive and early submission is considered the "golden rule" to avoid delays and denials.
- Why it Matters: Pre-authorization ensures that the service is covered by your benefit plan, is medically necessary, and is cost-effective.Without this approval, you may be held responsible for the entire bill.
- In-Network vs. Out-of-Network: Navigating Provider Networks Understanding your provider network is critical for managing costs.
- In-Network Providers: These are doctors, hospitals, and other healthcare providers who have contracts with your insurance company. Using in-network providers typically results in lower out-of-pocket costs because they have agreed-upon rates with your insurer.
- Out-of-Network Providers: These providers do not have contracts with your insurance company. If you use out-of-network providers, you will likely pay significantly more, or your insurance may not cover the services at all.
- What to Do: Before any appointment or procedure, confirm that all providers involved in your care are in-network. This includes not just your primary doctor or surgeon, but also anesthesiologists, radiologists, pathologists, and any labs or imaging centers. Even if your hospital is in-network, individual providers within that hospital might be out-of-network.
- The No Surprises Act: Federal protections under the No Surprises Act, which took effect in 2022, ban balance billing for out-of-network emergency care and for scheduled out-of-network services (like those from radiologists or anesthesiologists) at an in-network facility when you haven't been notified or provided consent. This act aims to protect patients from unexpected bills.However, it's still best practice to confirm network status whenever possible. You can learn more about these protections from official sources like the American College of Emergency Physicians' guide to the No Surprises Act.
- Deductibles, Co pays, Co insurance, and Out-of-Pocket Limits: Knowing Your Financial Responsibilities These terms define how much you pay for your healthcare.
- Deductible: This is the amount you must pay out of pocket for covered services before your health insurance plan starts to pay.For example, if you have a $2,000 deductible, you pay the first $2,000 of your medical bills before your insurance kicks in.
- Co-payment (Co-pay): A fixed amount you pay for a covered healthcare service after you've met your deductible. For example, you might pay a $30 co-pay for a doctor's visit.
- Co-insurance: Your share of the costs of a covered healthcare service, calculated as a percentage of the allowed amount for the service. For example, if your plan's allowed amount for a service is $100 and your co-insurance is 20%, you pay $20 (after meeting your deductible), and your insurer pays the remaining $80.
- Out-of-Pocket Limit (Maximum): This is the most you have to pay for covered services in a plan year. After you reach this limit, your health plan pays 100% of the costs for covered essential health benefits.This limit includes deductibles, co-payments, and co-insurance.
- What to Do: Review your Summary of Benefits and Coverage (SBC), which your insurer is required to provide, to understand these figures. This document helps you compare plans and understand your financial obligations. The Affordable Care Act (ACA) also provides protections related to these costs, such as ending lifetime and yearly dollar limits on essential health benefits.You can find more information on patient protections under the ACA on Healthcare.gov.
2. Document Everything

Maintaining meticulous records of all your healthcare interactions is one of the most powerful proactive steps you can take. If a denial does occur, a well-organized paper trail is invaluable. Counterforce Health's AI tools, for instance, are trained on thousands of real appeals and dissect your submitted documents line by line to identify inconsistencies and build strong arguments.
- What to Document:
- Appointments and Diagnoses: Keep a log of all doctor visits, including dates, names of providers, and the diagnoses discussed.
- Treatments and Medications: Record all prescribed treatments, medications (including dosage and frequency), and any procedures performed. Include details like physician's notes, ICD-10 diagnosis codes, CPT/HCPCS procedure codes, test findings, and any pertinent lab or imaging reports.
- Communications: Document every interaction with your healthcare providers and insurance company. This includes dates, times, names of people you spoke with, what was discussed, and any reference numbers provided. If possible, follow up phone calls with an email summarizing the conversation.
- Explanation of Benefits (EOBs) and Bills: Keep all EOBs and medical bills, even if they show a zero balance. These documents contain crucial information, including denial codes, which are essential if you need to appeal.
- Physician Orders: Ensure all physician orders for tests or services are signed and dated on or prior to the date of service. Verbal or telephone orders should be fully documented and countersigned by the ordering provider as soon as possible, but no later than 30 days after the order was given.Electronic signatures from the ordering provider are acceptable in electronic health records.
- Medical Necessity: All documentation should be specific to your situation, accurately reflect services performed, and clearly support the necessity for those services.Avoid "cloning" documentation, as it can misrepresent medical necessity.
- How to Organize and Submit Records:
- Legibility: Ensure all entries are legible. Poor handwriting or copy quality can render records unusable for review.
- Accuracy: Incomplete or inaccurate information is a leading cause of delays and denials.Double-check all demographic and insurance information.
- Submission: When submitting additional medical records in response to an insurer's request, electronic submission via portals like Availity is often recommended.If mailing or faxing, always include a copy of the request letter on top of the records.For unsolicited records, ensure a clear description of the billed code is included.
3. Decipher Your Policy

Insurance policies are notoriously complex, filled with jargon that can be confusing. Taking the time to understand key terms in your policy can help you identify potential pitfalls before they become issues.
- "Medically Necessary": The Subjective Standard This is a frequently used, yet often subjective, term. Insurers typically only cover services deemed "medically necessary." Understand how your plan defines this and ensure your doctor's documentation clearly justifies the necessity of your treatment. This is where detailed clinical documentation, including physician's notes and test findings, becomes crucial.
- "Experimental" or "Investigational": Challenging Unfair Labels Insurance companies sometimes deny FDA-approved treatments by labeling them as "experimental" or "investigational," even when they are legitimate and recommended by your doctor. Familiarize yourself with how your policy defines these terms and what criteria must be met for coverage. Counterforce Health specifically addresses how to challenge these types of denials.
- Exclusions and Limitations: Be aware of any specific services, conditions, or treatments that your policy explicitly excludes or limits. For example, some specified disease policies may only cover actual treatment for that disease and not related charges.Understanding these limitations upfront can prevent unexpected denials.
- Patient Rights and Protections: The Affordable Care Act (ACA) introduced significant patient protections that can help you navigate your policy. These include:
- Coverage for Pre-existing Conditions: Insurers cannot charge more or deny coverage based on pre-existing health conditions, including pregnancy.
- Preventive Care: Many preventive services are covered at no extra cost.
- Right to Appeal: You have the right to appeal a health plan decision.
- Choice of Doctors: The law protects your choice of doctors.
- No Frivolous Cancellations: It's illegal for health insurance companies to cancel your health insurance just because you get sick. You can find comprehensive information on these rights and protections on the U.S. Department of Labor's website regarding the ACA.
4. Partner with Your Physician

Your doctor is your primary advocate for your health, and they can also be a crucial partner in preventing denials. Physicians often spend considerable time battling insurance companies on behalf of patients. Empowering them to support your proactive efforts can be mutually beneficial.
- Clear Documentation and Justification: Encourage your physician to provide thorough and detailed documentation for your diagnosis, treatment plan, and the medical necessity of any procedures or medications. Proper coding (e.g., ICD-10 diagnosis codes, CPT/HCPCS procedure codes) and justification are paramount for preventing denials.
- Pre-Authorization Support: Your doctor's office is usually responsible for submitting pre-authorization requests.Follow up with them to ensure these are submitted promptly and correctly. They can leverage technology like integrated EHR/PM systems for efficient pre-authorization management.
- The Physician as Advocate: Physicians are increasingly taking on the role of patient advocates, helping to coordinate care, simplify complex medical information, and ensure patients' voices are heard.They can provide crucial supporting documents, such as letters of medical necessity, which are vital for a successful appeal if a denial does occur. Counterforce Health's tools are designed to empower physicians, allowing them to generate multiple appeals in a day and focus more on patient care.
- Understanding Patient Rights: As a patient, you have rights, including timely access to medical care, the right to easy-to-understand information about your diagnosis and treatment options, and the right to ask questions to make informed decisions.Your physician can help ensure these rights are upheld. You can review a comprehensive list of patient rights from the U.S. Department of State.
By taking these proactive steps, you empower yourself with knowledge and preparation, significantly reducing the likelihood of encountering a claim denial. While Counterforce Health stands ready to help you fight and win appeals when they happen, our ultimate goal is to help you focus on healing, not fighting. We believe that by working together, patients, providers, and advocates, we can transform a broken healthcare system into one that truly puts people first.
Read More: